| Definitions | Methodology | Classifications | Publications | Links | Contact |
Active tuberculosis a case of tuberculosis (TB) is defined as a patient in whom the treating physician has diagnosed any form of tuberculosis and initiated a course of therapy according to treatment guidelines.
Age group patients age in years on the day of tuberculosis diagnosis confirmation.
Confirmed TB cases bacteriological examinations positive sputum smear microscopy and/or culture positive for pulmonary TB and culture positive for extrapulmonary TB.
Extrapulmonary tuberculosis tuberculosis of organs other than the lungs, e.g. pleura, lymph nodes, abdomen, genito-urinary tract, skin, joints and bones, meninges. Patients with both pulmonary and extrapulmonary TB should be classified as a case of pulmonary TB.
ICD-10 international statistical classification of diseases and related health problems, tenth edition.
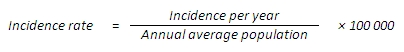
Incidence a process that indicates the rate of disease occurrence in the population. It is measured by: an absolute count a count of new incident cases or newly diagnosed cases per year; or by relative numbers usually rate per 100 000 population.
Incidence rate denotes the number of new cases (the final diagnosis confirmed for the first time in the life of a patient) of a disease in relation to the size of the population during a certain period. As a rule, this index is calculated per 100 000 people per year.
MDR or multidrug-resistance resistance to at least isoniazid and rifampicin.
New case a patient who has never had treatment for TB or who has taken antituberculosis drugs for less than 1 month.
Pulmonary tuberculosis tuberculosis involving only the lung parenchyma. Patients with both pulmonary and extrapulmonary TB should be classified as a case of pulmonary TB.
Relapse a patient previously treated for TB, declared cured or treatment completed, and who is diagnosed with bacteriological (+) TB (sputum smear microscopy or culture).
Treatment after lost to follow up a patient who returns to treatment, positive bacteriologically, following interruption of treatment for 2 or more consecutive months.
Treatment after failure a patient who is started on a re-treatment regimen after having failed previous treatment.
Treatment outcome definitions:
Cured patient who has completed treatment according to guidelines, who was sputum smear microscopy / culture positive at the beginning of the treatment and who was sputum negative in the last month of treatment and on at least one previous occasion.
Cured (for MDR cases) patient who has completed treatment according to guidelines and has at least 5 consecutive negative cultures from samples collected at least 30 days apart in the final 12 months of treatment.
Treatment completed patient who has completed treatment, but who does not meet the criteria to be classified as a cure (because of lack of bacteriological results) or a failure.
Treatment failure new patient who is sputum smear microscopy positive at 5 months or later during treatment, or who is switched to Category IV treatment because sputum turned out to be MDR TB. Previously-treated patient who is sputum smear microscopy positive at the end of his/her re-treatment or who is switched to Category IV treatment because sputum turned out to be MDR TB.
Treatment failure (for MDR cases) treatment will be considered to have failed if 2 or more of the 5 cultures in the final 12 months of therapy are positive or if any of one of the final three cultures is positive. Treatment will also be considered to be failed if a clinical decision has been made to terminate treatment because of poor clinical or radiological response or adverse events.
Died patient who dies from any cause during treatment.
Died due to other causes a patient has died during treatment due to other causes than tuberculosis.
Died due to tuberculosis a patient has died during treatment, and the cause of death is defined as tuberculosis.
Lost to follow up patient whose treatment was interrupted for 2 consecutive months or more without medical approval.
Transfer out patient who has been transferred to a health facility in another reporting and recording unit or for whom treatment outcome is not known.
Tuberculosis (causal microorganism: Mycobacterium tuberculosis) a dangerous infectious disease that may affect all organs and tissues. In 9095% of cases, the disease is expressed as pulmonary tuberculosis, which is the most infectious form of the disease due to spreading by droplet transmission.
XDR extensive drug-resistance (WHO definition until 2020) resistance to any fluoroquinolone and least one of the three injectable second line drugs (capreomycin, kanamycin and amikacin), in addition to multidrug-resistance.
XDR extensive drug-resistance (WHO definition from 2021) TB caused by Mycobacterium tuberculosis (M. tuberculosis) strains that fulfil the definition of MDR/RR-TB and which are also resistant to any fluoroquinolone and at least one additional Group A drug (Group A drugs are the most potent group of drugs in the ranking of second-line medicines for the treatment of drug-resistant forms of TB using longer treatment regimens and comprise levofloxacin, moxifloxacin, bedaquiline and linezolid).
Terminology is used according to WHO Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis (WHO 2008).
The Estonian Tuberculosis Register is kept for tuberculosis cases registering, tuberculosis prevention, tuberculosis incidence, prevalence and tuberculosis survival analysis, health care and tuberculosis control, health policy development, diagnostic and treatment assessment and statistics and scientific research, including epidemiological research.
Data providers for the Estonian Tuberculosis Register are all health care providers and Estonian Forensic Science Institute experts who diagnose tuberculosis cases in live patients and after death.
NB! In annual statistics, one treatment case per patient is taken into account.
Data is provided using the 10th edition of the International Classification of Diseases and Health-related problems (ICD-10).
More info is available at on WHO website or browse classification directly here https://icd.who.int/browse10/2019/en.
Classification of Administrative and Settlement Units of Estonia (EHAK)
This classification is used upon submission of regional statistics. Regional health care statistics are submitted by 15 counties. Information about Tallinn, Kohtla-Jδrve, Narva, Pδrnu and Tartu is submitted separately. Until 2017, data by the counties is distributed by the administrative division that existed before administrative reform (October 2017). Data starting from 2018 is distributed by new administrative division. This classification system is available on the webpage of the Statistics Estonia in the Classifications section.
Kasianczuk M, Rόόtel K, Tšerkašina E, Kulbayev S, Djuma V. Immigrants in Estonia: a risk assessment to involve the key group into HIV and co-infections services. Study Report. Tallinn: ECOM; 2021.
Hollo V, Villand K, Viiklepp P. Tuberkuloosihaigestumus Eestis 20142019. Tallinn: National Institute for Health Development; 2021.
Policy Brief: Empowering the Public Health System and Civil Society to Fight the Tuberculosis Epidemic among Vulnerable Groups. TUBIDU project; 2014.
Viiklepp P. Tuberkuloosihaigestumus Eestis 20122013. Tallinn: National Institute for Health Development; 2014.
Viiklepp P. Tuberkuloosihaigestumus Eestis 20082009. Tallinn: National Institute for Health Development; 2010.
WHO web for tuberculosis data
Piret Viiklepp
Estonian Tuberculosis Register
National Institute for Health Development
Phone: +372 5878 6531
E-mail: Piret.Viiklepp[at]tai.ee
Updated: 18.02.2026